Antiretroviral drugs (ARVs) were originally developed to treat people living with HIV. But research has proven that ARVs can also prevent HIV acquisition among individuals who are HIV-negative. This is called pre-exposure prophylaxis, or PrEP, and it’s a vital tool in HIV prevention.
PrEP Delivery
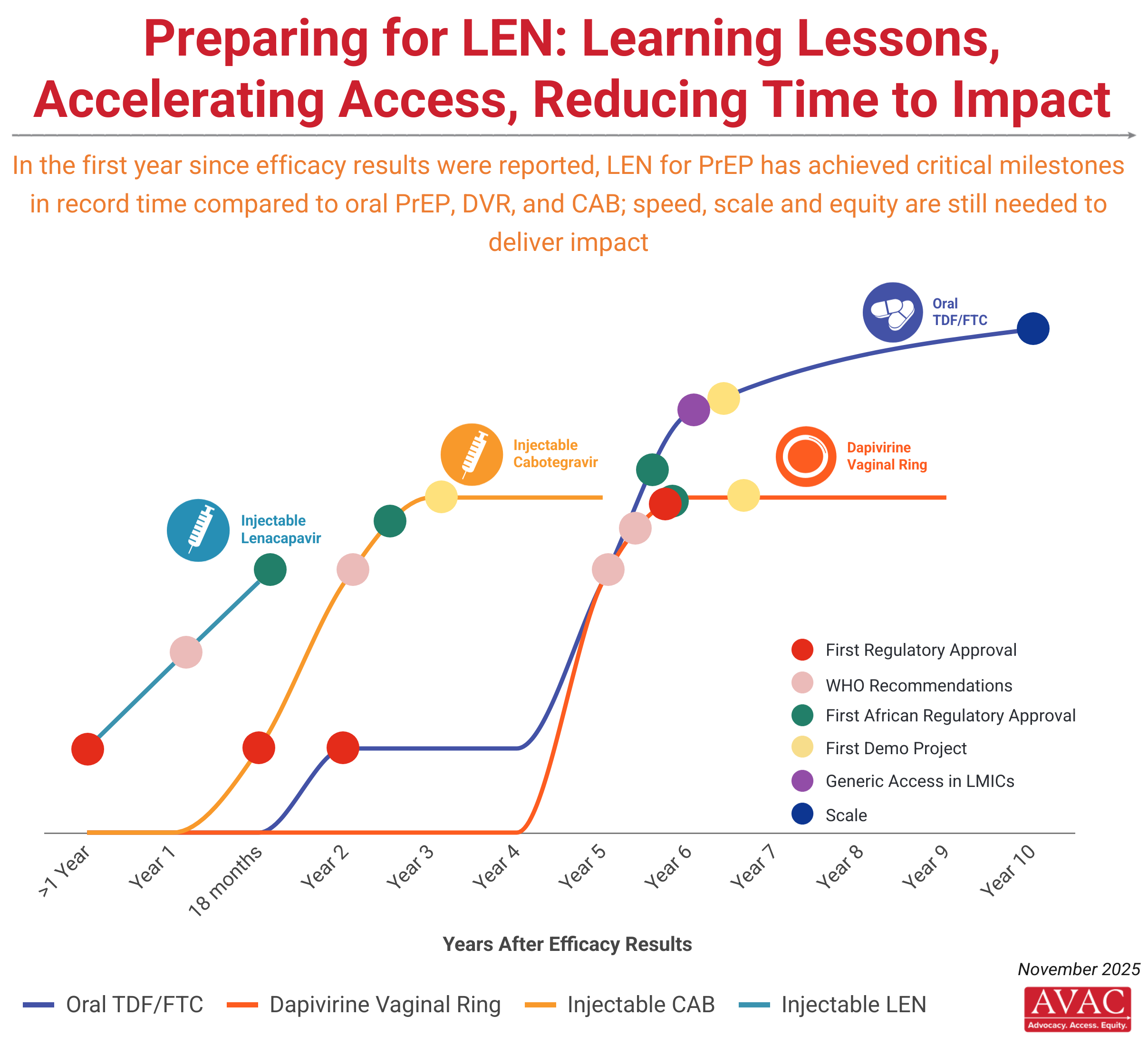
The first daily PrEP pill was approved by the FDA in 2012, but rollout was slow, uncoordinated and poorly planned. Uptake is nowhere near where it should be to address the HIV epidemic. (See the trends in AVAC’s PrEP Tracker). While PrEP won’t be right for everyone at risk, the next generation of products — some entering the market now — must act on the lessons from oral PrEP rollout, by improving coordination and speeding access.
The rollout of injectable lenacapavir (LEN for PrEP), injectable cabotegravir (CAB for PrEP) and the dapivirine vaginal ring (DVR), the latest prevention tools to be proven effective, represents an opportunity to get rollout right.
Approved Options
- Lenacapavir showed 100% efficacy in the PURPOSE 1 trial, and was approved by the FDA in June 2025. To learn all about lenacapavir and for related AVAC resources, click here.
- Cabotegravir became the first injectable PrEP option when it gained regulatory approval in 2021. Learn more about injectable CAB for PrEP on PrEPWatch.org
- The dapivirine vaginal ring received a positive opinion from the European Medicines Agency in 2020. Learn more about the ring on PrEPWatch.org
- F/TAF (brand name Descovy) became the second daily oral PrEP pill to be approved in 2019, but only for men who have sex with men (MSM) and transgender women. Efficacy studies of F/TAF among cisgender women are ongoing. Learn more about F/TAF and the current trial on PrEPWatch.org
- The daily pill TDF/FTC (brand name Truvada) was first approved for use as oral PrEP in 2012. Now dozens of countries have approved it and launched programs to deliver it. But PrEP still has not reached many of the people who need it most.
PrEP in Development: What’s in the pipeline?
Research and development for PrEP includes a diversity of products. Early phase development includes patches, gels, douches, implants, films, vaginal and rectal inserts, topical agents, long-acting and short-acting products. Further along in development are a monthly oral pill (MK-8527), a 3-monthly ring, a multi-purpose technology that combines PrEP with a contraceptive that prevents pregnancy (the Dual Prevention Pill), and a longer-acting injectable. To learn more about these products go to prepwatch.org/products.
PrEP Advocacy
Effective advocacy for smarter, better rollout of approved PrEP products remains essential, along with advocacy for continued investment in developing additional PrEP options.
AVAC supports a range of programs to advance this advocacy. We track the status of rollout and uptake of all approved PrEP products; call for continued investment in R&D for new options; support engagement between researchers, donors, community leaders, government and civil society in the design of trials investigating new PrEP options and the design of programs to deliver PrEP effectively to everyone who needs it; and participate in collaborations to hold decision-makers accountable to commitments on funding, policy and more so that prevention programs rolling out PrEP work in the real world.
Find out more about PrEP access and rollout across the globe at AVAC’s PrEPWatch.